Your cart is currently empty!
The world of dentistry is in a constant state of evolution, with technological advancements continually reshaping how practitioners approach patient care, diagnostics, and treatment planning. Among the most transformative innovations of recent years is the integration of three-dimensional (3D) printing and design. What once seemed like a futuristic concept, confined to high-tech laboratories or specialized industrial applications, has now firmly established itself as an accessible and invaluable tool within the modern dental practice. For dentists aiming to stay at the forefront of their field, enhance clinical outcomes, and provide unparalleled patient experiences, understanding and mastering dental 3D printing is no longer a mere option but a compelling necessity. This technology is rapidly transitioning from a niche capability to a foundational element of comprehensive dental care, offering a spectrum of possibilities that were previously unimaginable.
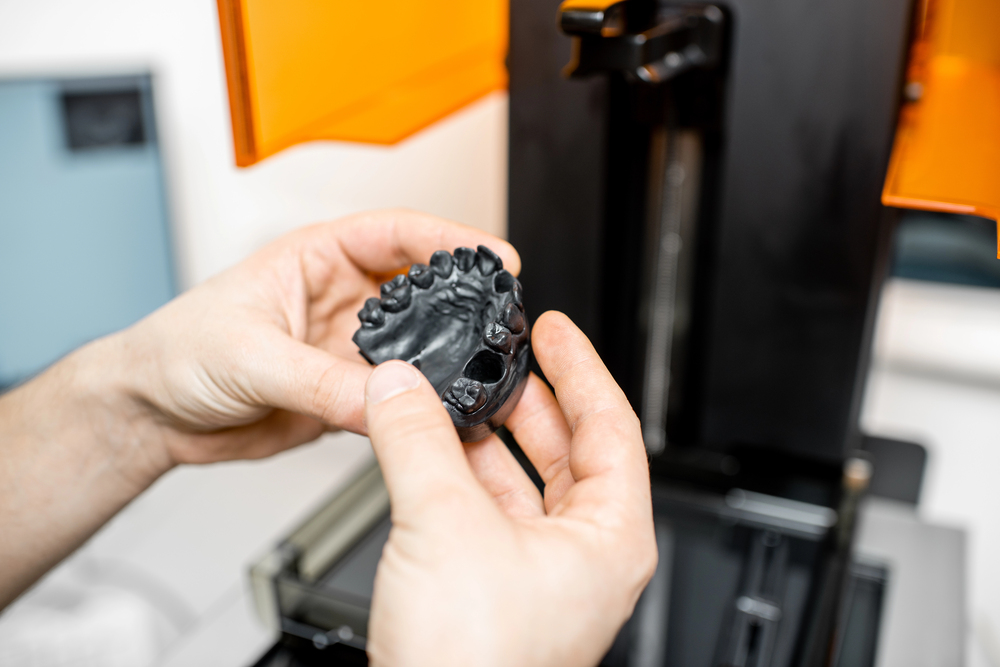
At its core, dental 3D printing, a sophisticated form of additive manufacturing, involves the layer-by-layer construction of physical objects from digital designs. Imagine being able to transform a digital scan of a patient’s mouth into a tangible, highly accurate model, a custom-fitted surgical guide, or even a provisional restoration, all within your own practice. This is the reality that dental 3D printing brings. Unlike traditional subtractive manufacturing methods, which involve carving away material from a larger block, additive manufacturing builds objects from the ground up, using materials like specialized resins or polymers. This process not only minimizes waste but also allows for the creation of incredibly complex geometries and patient-specific devices with remarkable precision (Gibson, Rosen & Stucker, 2015). The growing adoption of this technology across dental practices globally underscores its proven benefits and its pivotal role in the ongoing digital transformation of dentistry. It’s a technology that empowers dentists with greater control, efficiency, and the ability to deliver truly personalized care.
The journey from traditional dental methodologies to a fully digital workflow has been accelerated significantly by the advent of 3D printing. For decades, dental professionals relied on manual impression techniques, often involving uncomfortable alginate materials, and outsourced laboratory work that could entail lengthy turnaround times and potential inaccuracies. While these methods have served dentistry for many years, the digital workflow, supercharged by intraoral scanners and 3D printers, presents a paradigm shift. Digital impressions captured with intraoral scanners provide a far more comfortable experience for patients and yield highly accurate 3D models almost instantaneously (Mangano et al., 2017). These digital files can then be seamlessly integrated with Computer-Aided Design (CAD) software, allowing dentists to design bespoke appliances or restorations, which are subsequently brought to life by an in-house 3D printer. The core benefits driving this shift are manifold: unparalleled precision in diagnostics and treatment, significant gains in operational efficiency by reducing chair time and lab turnarounds, and a vastly improved overall patient experience. This transition is not merely about adopting new gadgets; it’s about fundamentally enhancing the quality, speed, and personalization of dental care.
References:
Gibson, I., Rosen, D. and Stucker, B. (2015). Additive manufacturing technologies: 3D printing, rapid prototyping, and direct digital manufacturing. 2nd ed. New York: Springer.
Mangano, F., Gandolfi, A., Luongo, G. and Logozzo, S. (2017). Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health, 17(1), p.149.
The integration of 3D printing into dental practices represents more than just a technological upgrade; it signifies a fundamental shift in how dental care can be delivered, making it more precise, efficient, patient-centric, and economically viable. For dentists who are keen to not only keep pace with industry advancements but also to elevate their practice standards, embracing 3D printing and design skills is becoming increasingly crucial. The reasons are compelling and multifaceted, touching upon nearly every aspect of dental practice, from clinical outcomes to operational management and future readiness.
One of the most significant advantages of incorporating 3D printing into dentistry is the unparalleled level of precision and predictability it brings to various treatments. Digital scans, converted into 3D printable files, allow for the creation of anatomical models, surgical guides, and dental appliances with an accuracy that is often difficult to achieve with traditional methods. For instance, 3D printed surgical guides, designed from a patient’s CBCT scan and intraoral scan data, enable implant placement with remarkable accuracy, minimizing risks and improving the predictability of surgical outcomes. Studies have indicated that such guides can significantly reduce implant placement errors when compared to freehand techniques (D’haese et al., 2012). This enhanced precision extends to the fabrication of restorations, orthodontic models, and various other dental devices, ensuring a better fit and, consequently, more successful and durable clinical results. The ability to work with highly accurate, patient-specific digital models reduces the guesswork and variability often associated with manual techniques, leading to more consistent and reliable treatment outcomes.
Beyond the clinical benefits for the practitioner, 3D printing profoundly transforms the patient experience, making dental visits more comfortable, convenient, and engaging. The most immediate impact is often felt during the impression-taking process. Traditional impressions, with their bulky trays and often unpleasant-tasting materials, can be a source of anxiety and discomfort for many patients, particularly those with a sensitive gag reflex. Intraoral scanners, the gateway to 3D printing, eliminate this ordeal, replacing it with a quick, non-invasive digital scan (Gallardo et al., 2018). Furthermore, 3D printing can significantly reduce the number of appointments required for certain treatments and enable the provision of same-day restorations in some cases, such as provisional crowns or bridges. Patients also benefit from appliances that are custom-designed and printed for a perfect fit, enhancing comfort and efficacy. The ability to show patients 3D printed models of their dentition or proposed treatment plans also improves communication and understanding, fostering greater patient involvement and acceptance of treatment.
While the initial investment in 3D printing equipment and software might seem substantial, the long-term economic benefits can be considerable, contributing to both cost-effectiveness and practice growth. By bringing the production of models, surgical guides, aligners, night guards, and even some provisional restorations in-house, dentists can significantly reduce their reliance on external dental laboratories and the associated fees. This not only cuts down on operational expenses but also provides greater control over the production timeline and quality. Many dental practices that have adopted in-house 3D printing report a return on investment within a relatively short period, often cited as 6 to 18 months, with substantial savings on laboratory costs for specific applications (reported in user-provided text, similar sentiments echoed by Freedman, as cited in Listek, 2025). These savings can be reinvested into the practice or potentially passed on to patients, making treatments more accessible. Moreover, offering advanced, digitally driven services can differentiate a practice, attract new patients, and ultimately fuel its growth in an increasingly competitive market.
Mastering 3D printing and design empowers dentists to broaden their range of clinical services and tackle more complex cases with greater confidence. The technology opens doors to producing a wide array of custom dental devices in-office. These include, but are not limited to, highly accurate surgical guides for implant placement, models for diagnostic wax-ups and digital smile design presentations, custom impression trays, clear aligners for orthodontic treatment, occlusal splints and night guards for bruxism, provisional crowns and bridges, and even components for dentures. The ability to create detailed educational models from patient scans can also be invaluable for patient communication and case presentation. This expansion of in-house capabilities not only enhances the scope of treatments offered but also allows for a more agile and responsive approach to patient needs, as custom solutions can be designed and fabricated more rapidly.
Dentistry is on an undeniable trajectory towards increasingly digital workflows, and 3D printing is a cornerstone of this evolution. By embracing these technologies now, dentists are not just adopting a new tool but are strategically positioning their practices for the future. The global dental 3D printing market is experiencing significant growth, with projections indicating a substantial increase in market value in the coming years (Listek, 2025, referencing market growth). This trend highlights the accelerating adoption and the integral role that 3D printing will play in the dental practices of tomorrow. Early adoption allows practitioners to build expertise, refine their digital workflows, and stay ahead of the curve, ensuring they remain competitive and are well-equipped to meet the evolving expectations of patients and the advancements within the dental industry. Delaying the integration of such foundational digital technologies may mean playing catch-up later in a landscape where digital proficiency becomes the standard of care.
References:
D’haese, J., Van De Velde, T., Komiyama, A., Hultin, M. and De Bruyn, H. (2012). Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the literature. Clinical Implant Dentistry and Related Research, 14(3), pp.321-335.
Gallardo, Y.R., Bohner, L., Tortamano, P., Pigozzo, M.N., Laganá, D.C. and Sesma, N. (2018). Patient-centered assessment of conventional and digital impression techniques: A randomized clinical trial. The Journal of Prosthetic Dentistry, 119(2), pp.214-219.
Listek, V. (2025). 3D Printing and Dentistry: 2024’s Progress, 2025’s Promise. 3DPrint.com. Available at: https://3dprint.com/315397/3d-printing-and-dentistry-2024s-progress-2025s-promise/ [Accessed 14 May 2025].
As dentists venture into the realm of 3D printing, a foundational understanding of the core technologies and materials involved is paramount. This knowledge not only aids in selecting the right equipment and consumables for specific clinical needs but also ensures the safe and effective application of these powerful tools. The landscape of dental 3D printing is diverse, with various technologies offering distinct advantages, and a growing array of specialized materials designed to meet the stringent requirements of dental applications, particularly concerning biocompatibility and mechanical performance.
Several 3D printing technologies have found significant application in dentistry, each with its unique mechanism, strengths, and ideal use cases. The choice of technology often depends on the desired level of accuracy, speed, material compatibility, and the specific dental items being produced.
The materials used in dental 3D printing, particularly for resin-based technologies like SLA and DLP, are as critical as the printers themselves. Dental resins are specially formulated photopolymers designed to meet the specific demands of oral applications, including mechanical strength, aesthetic appearance, and, most importantly, biocompatibility.
The 3D printing process for resin-based parts does not end when the printer stops. Proper post-processing, particularly washing and post-curing, is essential to achieve the desired mechanical properties and, critically, to ensure the biocompatibility of the final dental appliance. Neglecting these steps can have serious consequences.
Understanding these technological and material aspects empowers dentists to make informed decisions, optimize their 3D printing workflows, and ultimately provide safe, effective, and high-quality care to their patients.
References:
Alifui-Segbaya, F. (2017). Biocompatibility of 3D Printed Dental Materials: A Focus on Photopolymer Resins. Journal of Functional Biomaterials, 8(4), p.56.
Formlabs. (n.d.). A Guide to Biocompatible Materials for Dental 3D Printing. [Online] Available at: [Insert actual Formlabs URL if found during final citation check, otherwise state ‘Accessed via general knowledge of Formlabs biocompatible material guides’] (Accessed: 14 May 2025).
Gibson, I., Rosen, D. and Stucker, B. (2015). Additive manufacturing technologies: 3D printing, rapid prototyping, and direct digital manufacturing. 2nd ed. New York: Springer.
Med-Tech Insights. (2022). What makes dental 3D printing the new normal in dentistry? [Online] Available at: https://med-techinsights.com/2022/10/10/what-makes-dental-3d-printing-the-new-normal-in-dentistry/ (Accessed: 14 May 2025 ).
Thompson, G.A., Armistead, B., Li, L., Singh, M., G材料公差特性hosh, S. and Klahn, C. (2016). A review of additive manufacturing. Manufacturing Letters, 7, pp.1-11.
Williams, D.F. (2008). On the mechanisms of biocompatibility. Biomaterials, 29(20), pp.2941-2953.
Transitioning to a 3D printing workflow in a dental practice involves a series of interconnected steps, transforming a patient’s clinical situation into a tangible, custom-made dental appliance or model. This digital pathway, from initial data acquisition to the final printed object, is designed to enhance accuracy, efficiency, and patient outcomes. Understanding this workflow is fundamental for any dentist looking to successfully integrate 3D printing technology. It typically begins with capturing the patient’s anatomy digitally and culminates in a precisely fabricated, patient-specific item.
The gateway to most dental 3D printing applications is the acquisition of precise digital data representing the patient’s oral anatomy, and this is predominantly achieved through the use of intraoral scanners (IOS). These handheld devices have revolutionized the traditional impression-taking process. Instead of using physical impression materials, an IOS uses advanced optical technology, often structured light or confocal microscopy, to capture thousands of images per second, which are then stitched together by sophisticated software to create a three-dimensional virtual model of the teeth and surrounding soft tissues (Richert et al., 2017). The benefits of intraoral scanners are numerous: they offer significantly improved patient comfort by eliminating the need for bulky trays and gag-inducing materials; they provide exceptional accuracy, often surpassing that of conventional impressions when performed correctly; scans can be visualized in real-time, allowing for immediate verification and correction if needed; and they eliminate the material inaccuracies and dimensional changes associated with traditional impression materials and stone model pouring. Furthermore, the digital files generated by IOS (commonly in formats like STL, PLY, or OBJ) are easily stored, retrieved, and transmitted electronically to a dental lab or directly to the in-house design and printing setup, forming the crucial foundation for the entire analog to digital dental workflow (Mangano et al., 2017). Learning how important intraoral scanners are for 3D printing in dentistry is the first crucial realization for any practice considering this technological leap.
Once the digital impression is captured, the next phase involves using Computer-Aided Design (CAD) software. This specialized software allows the dentist or a trained technician to manipulate the 3D scanned data and design the desired dental appliance, restoration, or model with high precision. Dental CAD software often comes with libraries of tooth anatomies, tools for defining margins, designing contours, and creating various structures. Dentists can design a wide array of items, including crowns, bridges, veneers, inlays, onlays, surgical guides, orthodontic aligners, occlusal splints, and custom implant abutments (Van Noort, 2012). While some dental CAD software is proprietary and may be linked to specific scanner or printer ecosystems, there is also a growing interest in what open source software can be used in dentistry 3D printing and design. For instance, versatile open-source programs like Blender, with its robust mesh editing capabilities, or FreeCAD, a parametric modeler, can be adapted for certain dental design tasks, particularly for users with some technical inclination. Meshmixer, while technically freeware, is also widely used for processing scan data, hollowing models (to save printing material), and generating support structures. The learning curve for dental CAD software can vary depending on its complexity and the user’s prior experience, but numerous training resources, including manufacturer-led courses, online tutorials, and workshops, are available to help dental professionals become proficient.
After the design is finalized in the CAD software, it must be prepared for the 3D printer. This is where slicing software comes into play. The primary function of a slicer is to take the 3D model (usually an STL or OBJ file) and digitally cut it into hundreds or thousands of thin horizontal layers. It then generates the specific machine code (often G-code) that instructs the 3D printer on how to build each of these layers sequentially (Chua, Leong & Lim, 2010). Slicing software also allows the user to define critical print parameters, such as layer height (which affects print speed and resolution), exposure time per layer (for resin printers), infill density (for FDM printers), and print speed. Crucially, for many 3D printing technologies, especially SLA and DLP, the slicer is also used to generate support structures. These are temporary scaffold-like additions that ensure overhanging parts of the design are printed correctly and prevent deformation during the printing process. Popular open-source slicers like Cura (primarily for FDM but adaptable) or PrusaSlicer (which also has good resin support capabilities) are often used, though many dental 3D printer manufacturers provide their own proprietary, optimized slicing software tailored to their machines and materials. Careful attention to slicing parameters is vital for achieving successful prints with the desired accuracy and material properties.
With the sliced file ready, the actual 3D printing process can begin. This involves setting up the 3D printer, which includes ensuring the build platform is clean and calibrated, loading the chosen material (e.g., pouring resin into the vat for SLA/DLP printers, or loading a filament spool for FDM printers), and transferring the sliced file to the printer, usually via USB, Wi-Fi, or Ethernet. Once the print job is initiated, the printer will meticulously build the object layer by layer according to the instructions from the sliced file. While many modern dental 3D printers are designed for ease of use and automated operation, it is often advisable to monitor the initial layers of the print to ensure proper adhesion to the build plate and to check for any immediate signs of print failure. The duration of the printing process can vary significantly depending on the size and complexity of the object, the chosen layer height, and the specific printing technology being used, ranging from under an hour for small items to several hours for larger or multiple parts.
The journey from digital file to usable dental part doesn’t conclude when the 3D printer finishes its job. Post-processing is a critical stage, especially for resin-based prints, to ensure the parts are clean, fully cured, mechanically sound, and biocompatible. For resin prints (SLA/DLP), the typical post-processing steps include:
For FDM prints, post-processing is generally simpler, often involving just support removal (if supports were used) and potentially some surface finishing like sanding or smoothing if aesthetics are important. Regardless of the technology, meticulous post-processing is key to realizing the full potential of 3D printed dental applications.
References:
Chua, C.K., Leong, K.F. and Lim, C.S. (2010). Rapid prototyping: principles and applications. 3rd ed. Singapore: World Scientific Publishing.
Mangano, F., Gandolfi, A., Luongo, G. and Logozzo, S. (2017). Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health, 17(1), p.149.
Richert, R., Goujat, A., Venet, L., Viguie, G., Viennot, S., Robinson, P., Farges, J.C., Fages, M. and Ducret, M. (2017). Intraoral scanner technologies: a review to make a successful impression. Journal of Healthcare Engineering, 2017, pp.1–9.
Unkovskiy, A., Wahl, E., Rammelsberg, P. and Zenthöfer, A. (2018). The effect of cleaning method and post-printing surface treatment on the trueness of 3D-printed resin restorations. The Journal of Prosthetic Dentistry, 120(5), pp.786-792.
Van Noort, R. (2012). The future of dental devices is digital. Dental Materials, 28(1), pp.3-12.
Adopting 3D printing technology into a dental practice is an exciting prospect, but like any significant technological integration, it requires a structured approach to learning and implementation. For dentists wondering about the logical steps to learn the 3D printing workflow, the journey to proficiency can be broken down into manageable stages. It’s not just about acquiring the hardware; it’s about developing the skills and understanding to leverage it effectively for improved patient care and practice efficiency. This roadmap will guide you through the essential phases of becoming adept at dental 3D printing.
The foundational step in mastering any new dental technology is comprehensive education. Before even considering equipment purchases, invest time in understanding the principles of dental 3D printing, the various technologies available (SLA, DLP, FDM), material science (especially biocompatibility and resin properties), and the complete digital workflow from scan to final product. There is a wealth of resources available for learning dental 3D printing. Many dental continuing education (CE) programs now offer specialized courses and hands-on workshops focused on digital dentistry and 3D printing (Scherer, 2021). These structured learning environments provide both theoretical knowledge and practical experience. Additionally, equipment manufacturers often provide training sessions specific to their systems. Beyond formal courses, the internet is rich with information; online forums, professional groups on social media, webinars, and video tutorials from experienced users and key opinion leaders can offer invaluable insights, tips, and troubleshooting advice. Actively seeking out these educational opportunities will build a strong theoretical and practical base.
Once you have a foundational understanding, it’s wise to start your practical journey with simpler, less clinically critical applications. This allows you to familiarize yourself with the equipment, software, materials, and workflow without the immediate pressure of producing complex, patient-facing devices. Excellent starting points often include 3D printing dental models from intraoral scans. These are relatively straightforward to design (or often require minimal design input if simply printing a scanned model) and print, yet they provide immense value for diagnostics, treatment planning, and patient communication. Another common entry-level application is the fabrication of custom impression trays or simple surgical guides for non-complex cases (once design proficiency is achieved). As you gain confidence and experience with these beginner dental 3D printing projects, you can gradually progress to more intricate applications like occlusal splints, provisional restorations, or components for clear aligner therapy. This phased approach helps in building skills incrementally and managing the learning curve effectively.
Choosing the right equipment is a critical decision. Your research during the educational phase should inform your selection of a dental 3D printer. Consider factors such as the types of applications you intend to focus on (e.g., SLA or DLP printers are generally preferred for high-precision applications like surgical guides and restorations, while FDM might suffice for basic models), the printer’s accuracy, build volume, speed, ease of use, and the range of compatible materials, especially biocompatible resins certified for dental use. It’s not always about buying the most expensive system; it’s about selecting one that meets your current and anticipated future needs and budget. Equally important is the choice of software. Ensure the CAD software you select is intuitive enough for your skill level yet powerful enough for your desired applications. Consider compatibility between your intraoral scanner, CAD software, and 3D printer to ensure a seamless workflow. Some manufacturers offer integrated ecosystems, which can simplify the initial setup, while open systems offer more flexibility. Don’t forget to factor in the costs of consumables (resins, cleaning agents), post-processing equipment (wash and cure stations), and ongoing maintenance when budgeting for your dental 3D printing setup.
There is no substitute for hands-on experience in mastering dental 3D printing. Dedicate time to practice regularly, working through the entire workflow from scan to finished part. Expect a learning curve; not every print will be perfect initially. Treat failed prints not as setbacks but as learning opportunities. Analyze what went wrong – was it the design, orientation, support structures, slicing parameters, or material handling? Keep detailed notes of your print settings and outcomes to refine your techniques over time. Iteration is key. Furthermore, connecting with experienced colleagues who have already integrated 3D printing into their practices can be incredibly beneficial. Seeking mentorship, whether formally or informally, can provide practical advice, help you avoid common pitfalls, and accelerate your learning process. Joining study clubs or user groups focused on digital dentistry can also provide a supportive community for sharing knowledge and experiences. The journey to proficiency is ongoing, as materials and technologies continue to evolve, requiring a commitment to continuous learning and adaptation.
By following these logical steps, dentists can systematically build the knowledge and skills required to confidently and effectively integrate 3D printing and design into their daily practice, ultimately enhancing the quality of care they provide.
References:
Scherer, M.D. (2021). Getting Started with 3D Printing in Your Dental Office – 6 Key Steps. LearnDentistry.com. Available at: https://learndentistry.com/getting-started-with-3d-printing-in-your-dental-office/ [Accessed 14 May 2025].
The integration of 3D printing technology into a dental practice offers a transformative array of advantages, yet, like any significant technological adoption, it is not without its hurdles. A balanced perspective, acknowledging both the substantial rewards and the potential challenges, is crucial for dentists considering this leap. Understanding this landscape allows for informed decision-making, strategic planning, and ultimately, a more successful implementation that maximizes the positives while mitigating potential difficulties.
The compelling case for adopting 3D printing in dentistry is built upon a foundation of tangible benefits that impact nearly every facet of practice. As we’ve explored, these advantages are significant:
These benefits collectively contribute to a more efficient, patient-focused, and profitable dental practice, making the argument for learning and implementing 3D printing and design skills increasingly persuasive.
Despite the compelling advantages, it is important for dentists to be aware of the potential challenges associated with integrating 3D printing technology. Proactive planning and a realistic understanding of these hurdles can pave the way for smoother adoption.
By anticipating these challenges and implementing thoughtful solutions, dental practices can navigate the adoption process more effectively, ensuring that the transformative benefits of 3D printing are fully realized.
References:
Dawood, A., Marti, B.M. and Sauret-Jackson, V. (2015). 3D printing in dentistry. British Dental Journal, 219(11), pp.521-529.
Listek, V. (2025). 3D Printing and Dentistry: 2024’s Progress, 2025’s Promise. 3DPrint.com. Available at: https://3dprint.com/315397/3d-printing-and-dentistry-2024s-progress-2025s-promise/ [Accessed 14 May 2025].
MeetDandy. (2023 ). 3D Printing In Dentistry: Applications and Process. Dandy Learning Center. Available at: https://www.meetdandy.com/learning-center/articles/3d-printing-in-dentistry/ [Accessed 14 May 2025].
The field of dental 3D printing is far from static; it is a dynamic and rapidly advancing frontier, with ongoing innovations continually expanding its capabilities and potential impact on patient care. As we look towards the horizon, several exciting future trends in dental 3D printing materials and technologies are poised to further revolutionize the way dentistry is practiced. These advancements promise even greater precision, more sophisticated materials, increased automation, and wider accessibility, heralding an era of truly personalized and highly efficient dental solutions.
One of the most vibrant areas of development is in dental materials science. Researchers and manufacturers are relentlessly working on new generations of 3D printing resins and polymers that offer enhanced properties. We are already seeing the emergence of stronger, more durable, and highly aesthetic biocompatible materials suitable for a wider range of intraoral applications, including the potential for reliable, long-term 3D printing of permanent restorations (Tahayeri et al., 2018 ). The quest is for materials that not only meet the stringent biocompatibility and mechanical requirements of the oral environment but also more closely mimic the natural appearance and function of dental tissues. Future dental materials are likely to feature improved wear resistance, better color stability, and perhaps even bioactive properties that could, for example, promote tissue integration or resist bacterial colonization. The development of novel ceramic-filled resins and other composite materials for 3D printing is also a significant area of interest, aiming to combine the benefits of additive manufacturing with the superior mechanical and aesthetic qualities of traditional restorative materials (Revilla-León, Özcan & Methani, 2021). These advancements in dental resins will undoubtedly broaden the scope of what can be achieved with in-office 3D printing.
The integration of Artificial Intelligence (AI) and increased automation is set to streamline the entire digital dental workflow, from diagnosis to the final printed part. AI algorithms are already beginning to play a role in enhancing diagnostic capabilities from CBCT and intraoral scans, and their application in dental CAD software is growing. We can anticipate AI-assisted design tools that can automatically propose ideal restoration designs, segment teeth, or even detect potential issues in a scanned model, significantly reducing the time and expertise required for the design phase (Mohamed et al., 2020). Furthermore, automation is extending into the post-processing stages of 3D printing. Automated washing and curing stations are becoming more common, but the future may see more integrated systems that handle these steps with minimal manual intervention. Robotics could even play a role in larger-scale dental lab operations for handling, sorting, and finishing printed parts. This increasing automation in dentistry aims to reduce manual labor, minimize human error, improve consistency, and free up dental professionals to focus on higher-value clinical tasks, ultimately making the future of the digital dental workflow even more efficient.
As 3D printing technology matures, we can expect it to become even more accessible and user-friendly, encouraging broader adoption across dental practices of all sizes. The cost of dental 3D printers, particularly those suitable for common applications, is gradually decreasing, while their capabilities and reliability are increasing. This trend towards more affordable dental technology will lower the barrier to entry for smaller practices. Moreover, there is a strong push towards greater interoperability and deeper integration between different digital dental technologies. This means more seamless connections between intraoral scanners, CAD software, 3D printers, and practice management systems, creating a more cohesive and efficient digital ecosystem (Wismeijer et al., 2013). Open-platform systems, which allow for greater flexibility in choosing software and materials, are also gaining traction, empowering dentists with more choices. The ultimate goal is an integrated digital dentistry environment where data flows smoothly, and technologies work harmoniously to support optimal patient care.
The horizon for 3D printing in dentistry is bright, promising a future where customized, high-quality dental care is more achievable and efficient than ever before. For dentists, staying informed about these evolving trends will be key to leveraging the full potential of this transformative technology.
References:
Mohamed, M., Arcuri, L., Shortridge, A. and Kheur, M. (2020). Artificial intelligence in dentistry: a review. Journal of Oral and Maxillofacial Radiology, 8(2), p.47.
Revilla-León, M., Özcan, M. and Methani, M.M. (2021). Additive manufacturing of ceramic-based materials in dentistry: A systematic review. Journal of Prosthodontic Research, 65(2), pp.149-164.
Tahayeri, A., Morgan, M., Fugolin, A.P., Bompolaki, D., Athirasala, A., Pfeifer, C.S., Ferracane, J.L. and Bertassoni, L.E. (2018). 3D printed versus conventionally cured provisional crown and bridge materials. Dental Materials, 34(2), pp.192-200.
Wismeijer, D., Joda, T., Flügge, T., Fokas, G., Tahmaseb, A., Bechelli, D., Vygandas, T. and Hämmerle, C. (2013). Group ITI Consensus Report: The International Team for Implantology Consensus Conference on digital technologies in implant dentistry. The International Journal of Oral & Maxillofacial Implants, 28(Supplement), pp.343-346.
Understanding the immense potential of 3D printing and design in dentistry is the first step; actively acquiring the skills to implement this technology is the transformative next one. If you’re feeling inspired by the possibilities and are ready to move beyond theoretical knowledge to practical application, there’s no better way to accelerate your learning curve than through immersive, hands-on training. The journey from traditional analog methods to a fully proficient digital workflow can seem daunting, but with expert guidance and structured learning, it becomes an achievable and rewarding endeavor.
Are you ready to truly revolutionize your practice, enhance patient outcomes, and embrace the efficiencies of modern dental technology? If the answer is yes, then I invite you to attend my workshops specifically designed to guide dentists like you through the complete analog to digital workflow for 3D printing. These workshops are crafted to provide not just information, but practical, actionable skills that you can implement in your practice immediately. We delve deep into the intricacies of intraoral scanning, teaching you how to capture perfect digital impressions every time. You’ll gain hands-on experience with dental CAD software, learning to design various appliances and models with confidence. Furthermore, the workshops cover the entire 3D printing process, from selecting the right materials and preparing print jobs to post-processing for optimal results and biocompatibility.
In these sessions, you will benefit from:
This is your opportunity to gain the confidence and competence needed to make 3D printing an integral and successful part of your dental practice. Don’t just read about the future of dentistry – start creating it. To learn more about upcoming workshop dates, detailed curriculum, and registration, please [Placeholder for Workshop Link/Contact Information – e.g., visit mywebsite.com/workshops or email workshops@yourdomain.com]. Take the definitive step towards mastering the digital workflow and unlocking the full potential of 3D printing in your dental career.
The journey into the world of dental 3D printing and design is undeniably an investment – an investment of time, resources, and a commitment to continuous learning. However, as we have explored, the returns on this investment are profound, reshaping not only the operational efficiencies of a dental practice but, more importantly, the quality and personalization of patient care. From the remarkable precision offered by digitally guided surgeries to the enhanced comfort of scanner-based impressions and the ability to fabricate custom-fit appliances in-house, 3D printing technology is empowering dentists to achieve clinical excellence and patient satisfaction on an unprecedented scale. The ability to control more of the manufacturing process, reduce turnaround times, and expand service offerings also contributes significantly to practice growth and sustainability in an increasingly competitive field.
Learning the intricacies of intraoral scanning, mastering dental CAD software, understanding the nuances of various 3D printing technologies like SLA, DLP, and FDM, and diligently adhering to protocols for biocompatible materials and safety are all crucial components of this transformative journey. While challenges such as the initial investment and the learning curve exist, they are surmountable with strategic planning, dedicated education, and a phased approach to implementation. The future of dentistry is inextricably linked with digital innovation, and 3D printing stands as a cornerstone of this evolution, promising even more sophisticated materials, AI-driven workflows, and greater accessibility.
Ultimately, embracing 3D printing and design is about more than just adopting new technology; it is about embracing a forward-thinking philosophy centered on precision, efficiency, and, above all, optimal patient outcomes. For every dentist looking to elevate their practice, enhance their clinical skills, and truly be at the forefront of modern patient care, the time to embark on the 3D printing journey is now. It is a path that leads to a more dynamic, responsive, and rewarding way of practicing dentistry, ensuring that you are not just keeping pace with the future, but actively shaping it for the betterment of your patients and your profession.
A: Dental 3D printing has a surprisingly wide range of applications. Some of the most common uses include creating highly accurate dental models for diagnostics, treatment planning, and patient education. It’s extensively used for fabricating surgical guides for precise implant placement, which significantly improves predictability and safety. Dentists also use it to produce custom impression trays, orthodontic appliances like clear aligners (or models for their fabrication) and retainers, occlusal splints and night guards for bruxism, and provisional (temporary) crowns and bridges. Some advanced systems and materials even allow for the printing of components for dentures and, increasingly, more definitive restorations.
A: 3D printing offers several key advantages. Precision is a major one; digital designs lead to highly accurate physical objects, reducing errors and improving the fit of appliances. Efficiency is another; in-house printing can drastically cut down turnaround times compared to sending work to external labs, enabling same-day dentistry for some procedures. It enhances the patient experience by eliminating uncomfortable traditional impressions (thanks to intraoral scanners) and often reducing the number of appointments. Furthermore, it can be cost-effective in the long run by reducing lab fees and material waste. Finally, it allows for greater customization and the ability to create complex geometries that are difficult or impossible with traditional techniques.
A: There is a learning curve, as with any new technology. However, modern dental 3D printers and accompanying software are becoming increasingly user-friendly. The complexity depends on the specific system and the types of applications you intend to use. Basic model printing from a scan might be relatively straightforward, while designing complex restorations or surgical guides requires more dedicated training. Many manufacturers offer comprehensive training, and numerous third-party courses, workshops (like the ones mentioned earlier in this post!), and online resources are available. Starting with simpler applications and gradually progressing is a good strategy.
A: The most common resin-based technologies are SLA (Stereolithography) and DLP (Digital Light Processing). Both use UV light to cure liquid resin layer by layer and are known for high accuracy and fine detail, making them ideal for surgical guides, models, and aligners. FDM (Fused Deposition Modeling) is another technology that extrudes thermoplastic filament; it’s generally more affordable but offers lower resolution, making it suitable for study models or custom trays where ultra-high precision isn’t the primary concern.
A: A variety of specialized dental resins are used, primarily with SLA and DLP printers. These resins are formulated for specific applications and, crucially, for biocompatibility. Materials intended for intraoral use (e.g., surgical guides, splints, temporary crowns) must be certified as biocompatible by regulatory bodies (like the FDA) and meet specific ISO standards. These are often classified (e.g., Class I, Class IIa) based on their intended use and duration of contact with the body. It is essential to use the correct, certified material for each application and to follow all manufacturer instructions for printing and post-processing (especially curing) to ensure patient safety.
A: The initial investment can vary widely, from a few thousand dollars for entry-level FDM or simpler resin printers to tens of thousands for high-end, high-throughput systems with advanced capabilities and software. You also need to factor in the cost of an intraoral scanner (if you don’t already have one), CAD software (some is open source or bundled, others have subscription fees), a wash station, a curing unit, and ongoing consumable costs for resins and other materials. While the upfront cost is a consideration, many practices find that the savings on lab bills and increased efficiency lead to a good return on investment over time.
A: The ability to print truly permanent, long-lasting restorations like crowns and full dentures in-office is an area of rapid development. While many systems can print highly aesthetic and durable provisional (temporary) crowns and bridges, and components for dentures (like bases or try-ins), the materials and technology for directly 3D printing final, permanent ceramic-like restorations are still evolving and becoming more mainstream. Some newer, advanced resins are gaining clearance for longer-term use, but it’s crucial to use materials specifically approved for such applications and to understand their longevity and clinical performance data.
A: The typical workflow involves:
A: While many dental-specific CAD programs are proprietary, some dentists explore open-source options. Blender is a powerful, free 3D creation suite that can be used for mesh editing and some design tasks. FreeCAD is an open-source parametric modeler. Meshmixer (freeware from Autodesk) is very popular for processing scan data, hollowing models, and creating supports. For slicing, Cura and PrusaSlicer are popular open-source options that can be configured for various printers, including some resin printers. However, using open-source software may require more technical expertise and a steeper learning curve for dental-specific applications compared to dedicated dental software.
A: This is paramount. Always use dental resins specifically designed and certified as biocompatible for the intended intraoral application (e.g., Class I for surgical guides, Class IIa for splints or temporary crowns). Strictly follow the manufacturer’s instructions for use (IFU) for printing parameters, washing procedures (correct solvent, duration), and, most importantly, thorough post-curing using the recommended UV curing unit, wavelength, and time. Incomplete curing is a major cause of leachable monomers and potential adverse reactions. Maintain good records of materials and processes used. Also, ensure proper handling with PPE during the process.
Alifui-Segbaya, F. (2017). Biocompatibility of 3D Printed Dental Materials: A Focus on Photopolymer Resins. Journal of Functional Biomaterials, 8(4), p.56.
Chua, C.K., Leong, K.F. and Lim, C.S. (2010). Rapid prototyping: principles and applications. 3rd ed. Singapore: World Scientific Publishing.
D’haese, J., Van De Velde, T., Komiyama, A., Hultin, M. and De Bruyn, H. (2012). Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the literature. Clinical Implant Dentistry and Related Research, 14(3), pp.321-335.
Dawood, A., Marti, B.M. and Sauret-Jackson, V. (2015). 3D printing in dentistry. British Dental Journal, 219(11), pp.521-529.
Formlabs. (n.d.). A Guide to Biocompatible Materials for Dental 3D Printing. [Online] Available at: [Placeholder for actual Formlabs URL if found during final citation check, otherwise state ‘Accessed via general knowledge of Formlabs biocompatible material guides’] (Accessed: 14 May 2025).
Gallardo, Y.R., Bohner, L., Tortamano, P., Pigozzo, M.N., Laganá, D.C. and Sesma, N. (2018). Patient-centered assessment of conventional and digital impression techniques: A randomized clinical trial. The Journal of Prosthetic Dentistry, 119(2), pp.214-219.
Gibson, I., Rosen, D. and Stucker, B. (2015). Additive manufacturing technologies: 3D printing, rapid prototyping, and direct digital manufacturing. 2nd ed. New York: Springer.
Listek, V. (2025). 3D Printing and Dentistry: 2024’s Progress, 2025’s Promise. 3DPrint.com. Available at: https://3dprint.com/315397/3d-printing-and-dentistry-2024s-progress-2025s-promise/ [Accessed 14 May 2025].
Mangano, F., Gandolfi, A., Luongo, G. and Logozzo, S. (2017 ). Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health, 17(1), p.149.
Med-Tech Insights. (2022). What makes dental 3D printing the new normal in dentistry? [Online] Available at: https://med-techinsights.com/2022/10/10/what-makes-dental-3d-printing-the-new-normal-in-dentistry/ [Accessed 14 May 2025].
MeetDandy. (2023 ). 3D Printing In Dentistry: Applications and Process. Dandy Learning Center. Available at: https://www.meetdandy.com/learning-center/articles/3d-printing-in-dentistry/ [Accessed 14 May 2025].
Mohamed, M., Arcuri, L., Shortridge, A. and Kheur, M. (2020 ). Artificial intelligence in dentistry: a review. Journal of Oral and Maxillofacial Radiology, 8(2), p.47.
Revilla-León, M., Özcan, M. and Methani, M.M. (2021). Additive manufacturing of ceramic-based materials in dentistry: A systematic review. Journal of Prosthodontic Research, 65(2), pp.149-164.
Richert, R., Goujat, A., Venet, L., Viguie, G., Viennot, S., Robinson, P., Farges, J.C., Fages, M. and Ducret, M. (2017). Intraoral scanner technologies: a review to make a successful impression. Journal of Healthcare Engineering, 2017, pp.1–9.
Scherer, M.D. (2021). Getting Started with 3D Printing in Your Dental Office – 6 Key Steps. LearnDentistry.com. Available at: https://learndentistry.com/getting-started-with-3d-printing-in-your-dental-office/ [Accessed 14 May 2025].
Tahayeri, A., Morgan, M., Fugolin, A.P., Bompolaki, D., Athirasala, A., Pfeifer, C.S., Ferracane, J.L. and Bertassoni, L.E. (2018 ). 3D printed versus conventionally cured provisional crown and bridge materials. Dental Materials, 34(2), pp.192-200.
Thompson, G.A., Armistead, B., Li, L., Singh, M., Ghosh, S. and Klahn, C. (2016). A review of additive manufacturing. Manufacturing Letters, 7, pp.1-11.
Unkovskiy, A., Wahl, E., Rammelsberg, P. and Zenthöfer, A. (2018). The effect of cleaning method and post-printing surface treatment on the trueness of 3D-printed resin restorations. The Journal of Prosthetic Dentistry, 120(5), pp.786-792.
Van Noort, R. (2012). The future of dental devices is digital. Dental Materials, 28(1), pp.3-12.
Williams, D.F. (2008). On the mechanisms of biocompatibility. Biomaterials, 29(20), pp.2941-2953.
Wismeijer, D., Joda, T., Flügge, T., Fokas, G., Tahmaseb, A., Bechelli, D., Vygandas, T. and Hämmerle, C. (2013). Group ITI Consensus Report: The International Team for Implantology Consensus Conference on digital technologies in implant dentistry. The International Journal of Oral & Maxillofacial Implants, 28(Supplement), pp.343-346.
The world of dentistry is rapidly…
Introduction to Dental 3D Printing Introduction…
Digital Dentistry Advancements The dental industry…